IRANDERMA |
|
Quiz: June 2006 |
A 48-years-old man presented with a long-time history for an asymptomatic solitary tumoral lesion on his lower leg. He had manipulated the lesions with some caustic agents. Otherwise he was healthy.
What is your diagnosis ?

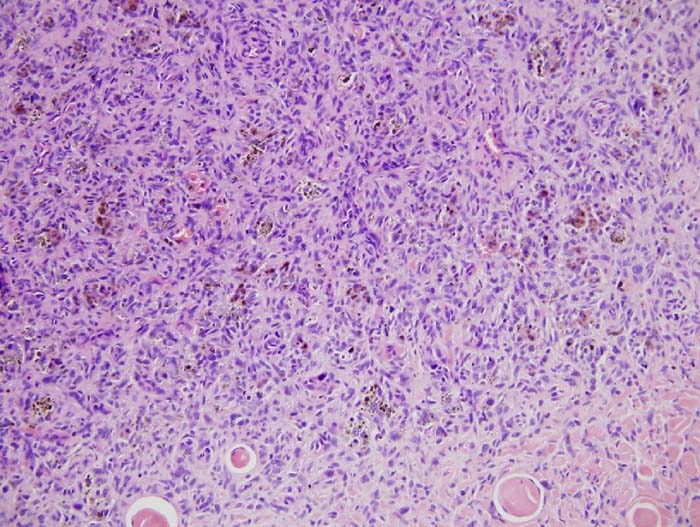
Diagnosis: Dermatofibroma; hemosiderotic type
O. Zargari: It should be kept in mind that hemosiderotic variant of dermatofibroma may be confused with pigmented lesions including blue nevus. Interestingly this issue has been addressed in a recently published paper;
Homogeneous blue pigmentation in dermatofibroma simulating a blue naevus.
J Eur Acad Dermatol Venereol. 2006 Jul;20(6):733-4
Below, you can read the opinions of the iranderma members about this disease;
Dr. Mehrdad Mehravaran, Szeged, Hungary
-
Synonyms: fibrohistiocytoma, nodular subepidermal fibrosis, histiocytoma cutis and sclerosing hemangioma.Dermatofibroma is a common fibrohistiocytic tumor, it occur as papules or nodules on the extremities in approximately 80% of cases.
The legs of women are a common location, possibly as a result of shaving or other minor trauma, and there are reports of cases involving the palms and soles. Although they have been reported to occur at any age, dermatofibromas most frequantly affect individuals in early to middle adult life (as in this case).
There is no racial predilection. Although usually solitary, in about 20% of patients multiple lesions will be found, and there are reports of generalized dermatofibromas, especially in immunosuppressed patients.
Dermatofibroma begins as a dusky red macule that quickly becomes a papule composed mostly of granulation tissue in company with innumerable extravasated erythrocytes within the dermis. Soon macrophages appear in abundance, and by ingestion of components of blood acquire the attributes of siderophages and lipophages. The lesion may become nodular and even tumorous, and progressively more firm as a consequence of production of altered collagen by proliferating fibrocytes. In time, fibroplasia predominates over granulomatous inflammation, and as more melanin is formed within the epidermis, the hard, dome-shaped lesion becomes browner. In time, after many years, the lesion slowly flattens consequent to shrinkage by fibroplasia. Sometimes the shrinkage is so great that the lesion at last is a hyperpigmented dell (as in this case).Differential diagnosis
Includes scar, keloids, xanthomas, neurofibromas, kaposi’s sarcoma, atypical nevus, and melanoma. A simple maneuver to help confirm the diagnosis can be done by applying lateral compression, which causes the central portion of the dermatofibroma to “dimple”. Larger lesions that extends into the fat and are several centimeters in diameter may be confused with dermatofibrosarcoma protuberans.Histopathology
Dermatofibromas are usually well circumscribed nodules confined to the dermis, measuring 1-2 cm in diameter and composed of plump fibroblasts arranged as intersecting fasicles. The likely cell of origin is the dermal dendrocyte. There are variable proportions of mononucleated and multinucleated foamy histiocytes, with hemosiderin deposits in their cytoplasm. Scattered between the cells, and predominantly at the periphery of the lesion, are thick “keloidal” collagen bundles that are birefringent when examined with polarizing lenses. Additional features are epidermal hyperplasia and a perivascular lymphoplasmacytic infilterate at the periphery of the nodule.Treatment
None, unless a lesion grows to several centimeters in diameter, when simple surgical excision may be indicated.
ايران درما |